Abstract
Background: Indefinite maintenance therapy after autologous stem cell transplant (ASCT) is the current standard of care in multiple myeloma (MM). However, in the real world, patients often discontinue treatment due to various reasons. In this study, we sought to analyze the effect of and reasons for early discontinuation of maintenance therapy on survival outcomes, studying patients who received less than 3 years of maintenance therapy (short-term maintenance group) or more than 3 years (continuous maintenance group).
Methods: We retrospectively reviewed 340 patients who underwent ASCT from 2005-2016 and received maintenance therapy for at least six months without progression. The patients started maintenance therapy after 100 days of ASCT. Lenalidomide (89%) and bortezomib (10%) were the most commonly used agents for maintenance therapy. The primary endpoints included were progression-free survival (PFS) and overall survival (OS). All the endpoints were measured from the time of ASCT. The discontinuation was defined as permanently stopping the maintenance therapy. Patient, disease, and transplant-related characteristics were compared between the two groups using the Mann-Whitney U test for continuous variables, and chi-squared or Fisher's exact test for categorical variables. The probabilities of PFS and OS were calculated using the Kaplan-Meier (KM) method and compared using log-rank test.
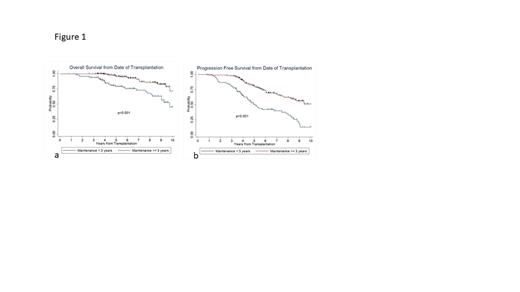
Results: One hundred and two (n= 102; 30%) patients discontinued maintenance therapy in the first 3 years (short-term maintenance group), while 238 patients remained on maintenance therapy for ≥ 3 years (continuous maintenance group). The groups had similar baseline characteristics in terms of age, gender, ISS staging, cytogenetics, response before ASCT, and melphalan dosing. About 20% of patients in both groups were older than 65 years. Among those alive at the last contact, the median follow up were 5.4 years and 6.1 years for the short-term and continuous maintenance therapy group, respectively. At the time of the last follow-up, 131/238 (55%) patients in the continuous maintenance group were still on maintenance therapy. The median PFS in the short-term maintenance group was 5.1 years (95% CI: 4.4-7.4) and median OS was 9.8 years (95% CI: 8.2- to NR), whereas in the continuous maintenance group both median PFS (95% CI: 8.5- NR) and OS were not reached. This latter group had significantly longer PFS and OS than the short-term maintenance group with a 5-year estimated PFS of 80% (95%CI: 74-85%) vs. 50% (95% CI: 39-60%) (p<0.001) and OS of 96% (95% CI: 92-98%) vs. 79% (95% CI: 69-86%) (p<0.001) (Figure 1). This remained significant after adjusting for race, post-transplant remission status and ISS staging, with an hazard ratio for risk of relapse or death of 0.31, 95% CI: 0.21-0.45; and HR for risk of death of 0.34, 95% CI: 0.18-0.64.
The most common reasons for early discontinuation of maintenance therapy (< 3 years) were adverse events related to maintenance therapy (58%). Four patient (4%) patients developed second primary malignancy (SPM) in this group. The most frequent hematological adverse events (AEs) were pancytopenia and isolated neutropenia. Fatigue and diarrhea were the most common non-hematological AEs. The reasons for stopping maintenance in the continued maintenance group were disease progression (24%) and adverse events (14%), while five patients (2%) developed SPM.
Conclusion: In our institutional experience, 30 percent of MM patients discontinued maintenance therapy within 3 years of ASCT due to AEs or patient preference. These patients had inferior PFS and OS after ASCT compared to patients on continuous maintenance. Therefore, continuation of maintenance therapy should be strongly encouraged as safely possible and strategies like dose reduction or switching therapy are recommended.
Bumma: Janssen: Membership on an entity's Board of Directors or advisory committees; Amgen: Speakers Bureau; Sanofi: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal